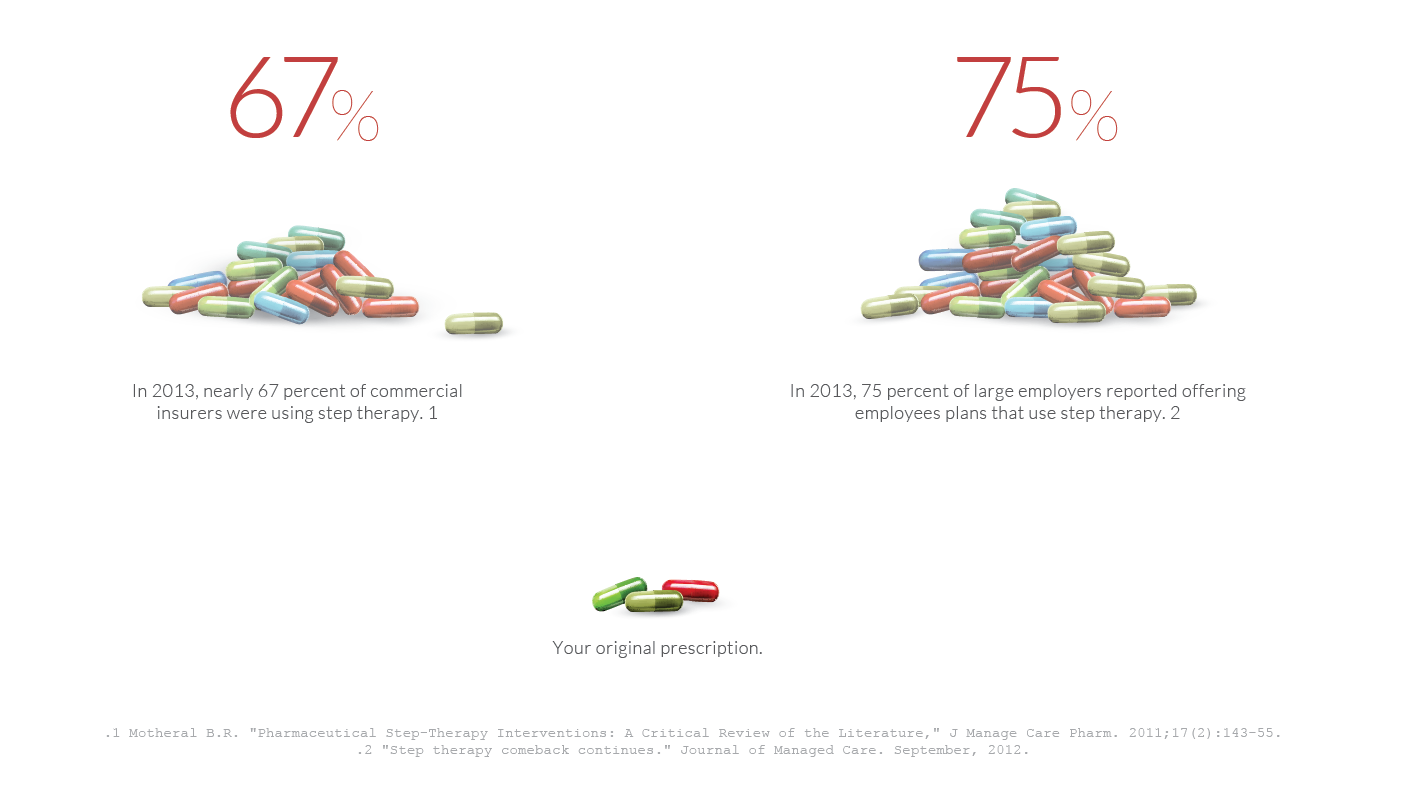
Fail First policies — also known as Step Therapy — are often insurance practices which require patients to fail on the insurer’s preferred drug, or drugs, before a patient can take the drug originally prescribed. Sometimes the preferred drugs are cheaper to the patient and sometimes they are not. Insurers can make a higher profit on the drugs they force patients to step through, and this is sometimes why they implement the policy. , Other times, fail first represents a generic drug which can be cheaper for the patient and less profitable for the insurer. However, your physician should make this decision, not your health insurance company.
When a patient has to fail first on a drug before being allowed to take the medication originally prescribed, the patient, physician and public health suffers.
This practice can result in serious negative consequences for consumers and the public health system. By limiting the medication options, both doctors and patients are forced to compromise their treatment decisions in a way that is dangerous, time consuming and more expensive in the long-term.
Often, when a patient’s insurance changes, the new company requires the fail first process to start again. With no limitations, fail first wreaks havoc on the lives of patients with chronic disease and their providers.